Introduction
Congenital dyserythropoietic anemias (CDA) are a rare group of hereditary disorders characterized by anemia, ineffective erythropoiesis, and secondary hemochromatosis. While some CDA patients respond to interferon α therapy (type I CDA) or splenectomy (type II CDA), others are dependent on chronic red cell transfusions lifelong. Hematopoietic cell transplant (HCT), remains the only curative option for this disease. In 39 patients reviewed by the European Society for Blood and Marrow Transplant (EBMT), graft rejection (GR) was 12% (1-23%), the 3-year overall survival (OS) and event free survival (EFS) were 71% (55-87%) and 45% (45-63%) respectively1. A trend towards higher incidence of GR and severe (Grade III-IV) acute graft versus host disease (GvHD) was observed in patients with iron overload and unrelated donor HCT but these risk factors were not statistically significant1. We report the outcomes in 17 children with CDA who underwent HCT at participating Pediatric Transplantation and Cellular Therapy Consortium (PTCTC) centers.
Methods
Clinical information on transplant and associated outcomes were collected retrospectively after IRB approval using a common questionnaire. Data were analyzed using descriptive statistics. Comparisons between groups were made using Fisher's exact tests. Survival estimates and corresponding 95% confidence intervals were performed using the Kaplan-Meier method.
Results
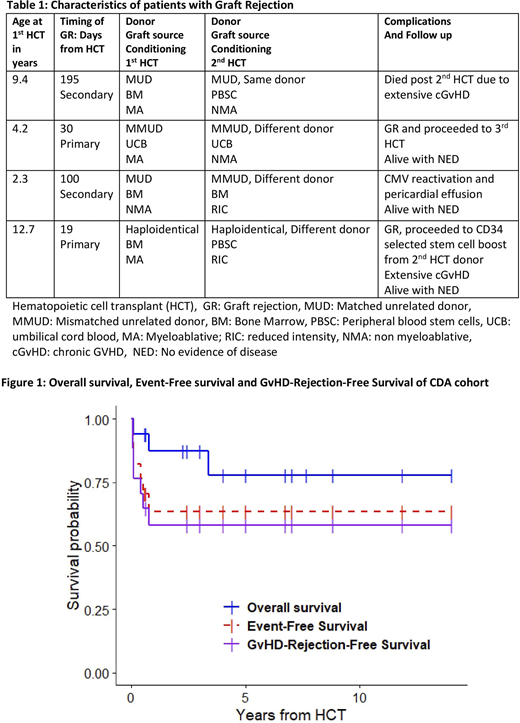
Seventeen patients (11 males) with CDA were eligible by diagnosis and underwent HCT from 2002-2019. The median age at diagnosis was 0.7 (range: 0.2 - 14) years. A majority (n=12) of patients had CDA type II while the remainder either had CDA type I (n=2) or were unknown (n=3). Twelve (71%) patients had evidence of iron overload by biopsy or imaging and 11 received pre-HCT chelation. Three of the 12 patients had liver fibrosis confirmed by biopsy. Thirteen patients had splenomegaly and four underwent splenectomy prior to HCT. Three patients received pre-HCT immunosuppressive therapy (PTIS). Median age at the time of HCT was 5.5 (range: 0.7 - 15) years. The median interval between diagnosis and HCT was 3.8 (range 0 - 12.3) years. Most patients received myeloablative busulfan-based conditioning (n=12); however, 5 patients received nonmyeloablative (n=1) or reduced intensity (n=4) fludarabine-based conditioning regimens. Donor sources included HLA matched sibling (n=3), matched unrelated (n=9), haploidentical (n=1) and mismatched unrelated (n=4) donors. Graft source was bone marrow in all but 2 patients who received umbilical cord blood. The median total nucleated cell (TNC) dose for bone marrow grafts was 6.0 (range: 3.4- 20.6) x 108/kg. Cord blood recipients received a TNC dose of 3.8 x 107 and 4.8 x 107/kg. Five (29%) patients developed acute GvHD grade II-IV, with one patient with grade III-IV acute GvHD (5.8%). Post-HCT complications included veno-occlusive disease (n=3), acute kidney injury (n=1), congestive cardiac failure (n=1), thrombotic microangiopathy (n=1), CMV viremia requiring therapy (n=2), mucormycosis (n=1), streptococcal pneumonia (n=1), recurrent clostridium difficle colitis (n=1), and parvovirus infection (n=1). Four patients developed chronic GvHD (23.5%; 2 limited and 2 extensive). Characteristics and outcomes of the four patients (23.5%) who developed GR are shown in Table 1. With a median follow-up of 3.4 (range: 0.08 - 14) years; fourteen patients are alive. Three patients died from respiratory failure due to adenovirus, congestive cardiac failure and extensive chronic GvHD post 2nd HCT. The 2-year OS, EFS and GvHD-free-rejection-free survival of the entire cohort (95% confidence interval) were 87% (72-100%), 64% (44 -92%), and 58% (39- 88%), respectively (Figure 1). Due to limited sample size, we did not find any patient or HCT-related factors that were associated with GR, OS or GvHD.
Conclusion
HCT can be curative for patients with CDA. The incidence of GR and GvHD in our CDA cohort was comparable to the recent EBMT report1. Strategies such as aggressive chelation, use of PTIS and perhaps early HCT in the presence of a suitable donor before co-morbidities occur are needed to improve engraftment without increasing risk for toxicities and mortality. Not unexpectedly we observed considerable morbidities in patients who had GR and required a 2nd HCT.
Pulsipher:Novartis: Honoraria; Bellicum: Honoraria; Jasper: Honoraria; Mesoblast: Honoraria; Miltenyi: Honoraria, Research Funding; Adaptive: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal